Not Just Cuddling Puppies and Kittens
Courtesy of: Joye
As a Registered Veterinary Technician, I often hear comments like “It must be nice to play with pets all day”, or “You have my dream job, hanging out with kittens and puppies!” Although on occasion we do get to share some special moments of cuddling with the amazing pets who come to see us, there are many hazards in the veterinary profession as well. Last week I experienced something that is one of the greatest fears in our profession…a dog bite on my face.
As members of the veterinary team, we accept that there are many risks in our line of work. Pets aren’t able to understand what we are doing to them, they are in a strange environment, and often times (from their perspective) we aren’t being very nice. We don’t respect their personal space and boundaries, and as a result we need to take many precautions to prevent injury to anyone (vet team, owners or pets) when pets become upset.
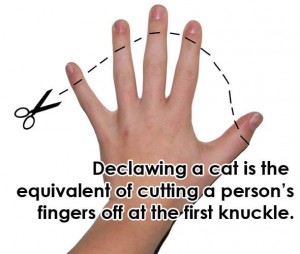
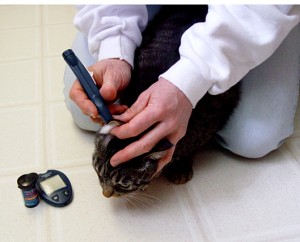
All of us have experienced some minor injuries in our line of work. Even a simple appointment such as vaccines for a new puppy can sometimes result in ugly scratches from sharp puppy nails. Cats come equipped with lots of built-in weapons and often aren’t afraid to show their displeasure with both their teeth and their claws. Many of these cats are happy house pets who wouldn’t scratch or bite in their own environment, but when they are subjected to strange people, smells, sights and sounds, all bets are off. We also work with feral (wild) cats who are trapped and brought in to be spayed or neutered and re-released. We expect these cats to be frightened and aggressive and we take precautions accordingly.
As with cats, some dogs find visiting our hospital extremely stressful. Dogs are generally much better at giving us warning signs when we are pushing them too far. They will often start either by avoiding our gaze or by directly staring at us. We also watch for what is called “whale eye“, when the white part of the eye is easily visible. These are early signs that a dog is uncomfortable in a situation. They may then escalate to a growl or a slight lift of their lips to show their teeth. If we continue our activities without paying attention to these signs, these dogs may bite. Some dogs who have a history of stressful visits to the vet may simply skip the preliminary warnings, however, and head straight to biting to get their point across.
We are very committed to protecting the safety of our team members, clients and patients. We have Occupational Health and Safety rules in place to provide guidance regarding handling these types of situations. Communication and awareness are key factors in keeping our hospital team safe. We have a system by which pet files are clearly marked with “Caution” stickers if the pet has a history of attempting to harm team members in the past. These stickers also include helpful information such as what methods of restraint worked best (for instance, some cats respond well to just being wrapped in a towel while some also benefit from an Elizabethan collar).
With dogs we record the type and size of muzzle we have used in the past. It is important that we all know the history of an animal before it comes into the exam room and each time we add notes about what methods are most successful.
Even with all these measures in place, unpredictable events occur. A dog who has only been mildly nervous in the past may suddenly become very defensive if they have to wait for a long time for their visit, or if there are other dogs in the waiting area that are feeling stressed. There may be strange smells in the hospital that day that are upsetting to dogs or cats. Hospital team members may be feeling rushed or pressured to get an appointment done quickly for a dog with a history of having a hard time at the vet, in an attempt to get them home and happy as quickly as possible. All of these factors may result in the nervous dog becoming a fearful dog, and fearful dogs are much more likely to bite.
Dog bite wounds are very rare in our hospital, thanks to our experienced team and good communication. Minor bites on the arms and legs are certainly serious concerns, but many people who work in our industry carry a little worry in the back of their mind about experiencing a bite on their face. In addition to permanent facial scarring, there is always a risk of damage to the eyes, which could be life altering. Thankfully, my eyes were unaffected, but my upper lip was torn and I have a large U-shaped laceration on my cheek. These required repair by a plastic surgeon and it may be months before we know how well the scars will heal.
Our team will be meeting to discuss this incident and look for ways to prevent something like this from happening again. While we continuously look for new ways to improve our safety at work, there are many things pet owners can do to help. Dogs and cats who are well socialized and frequently exposed to new situations in a safe manner are much more likely to handle vet visits well. If your dog has been nervous about visiting the vet in the past, consider dropping by for more frequent visits to allow team members to pet, play with and reward your dog when no negative procedures need to be done. Check out this great blog by Dr. Sophia Yin regarding Dog Bite Prevention Week, held annually in May, for more information. If your pet has a history of biting or showing defensive behaviours, it is important to let us know before your appointment so we can be prepared. Dr. Yin also has a blog about handling a dog who has bitten someone in the past, you can read it here.
Please respect our experience and best intentions when handling your pet. Even though your dog or cat may be friendly and happy with everyone at home, please trust us when we express concern over how they are feeling here. In some cases we may suggest that our technicians and assistants hold your pet for procedures, when we are concerned that the pet is stressed and may bite. We have all had training in recognizing the early warning signs discussed above. When we suggest that your dog may need a muzzle for procedures here, we aren’t trying to be mean to your pet, we are simply trying to keep everyone involved safe. If we work together, combining your knowledge of your pet’s normal behaviour with our experience and training, we can have every visit be safe and successful.
If you have any questions or concerns about how your pet handles vet visits, please call us at 902-893-2341. The suggestions above are merely the tip of the iceberg when it comes to making trips to the vet more relaxed and safer for your pets.